Survey finds patients want to talk about coverage and payment options before receiving care, but say providers aren’t initiating those discussions.
CHARLOTTE, N.C. – Dec. 16, 2020 – Two-thirds of consumers are concerned about their ability to pay for their medical expenses in 2021 given the financial pressures of the pandemic, according to a recent survey commissioned by AccessOne, a leading provider of patient financing solutions designed to help consumers better manage their healthcare costs.
Survey results show that Americans are feeling the economic strain of the COVID-19 pandemic, and it is impacting their medical decisions. The survey also found that half of consumers are likely to switch healthcare providers for access to 0% or low-interest payment plans—up from two-in-five consumers in AccessOne’s 2019 survey.
“Given the level of economic uncertainty and increased health risks presented by the pandemic, 2020 has been a challenging year for patients and providers alike,” said Mark Spinner, CEO for AccessOne. “Patients are continuing to delay medical care not just to limit their exposure to the virus, but also for financial reasons. Many consumers don’t fully understand their health insurance benefits, and healthcare leaders are focusing on ways to close that transparency gap to both promote trust and enable access and affordability.”
Key findings from the survey include the following:
- About half of consumers said they would be concerned about their ability to pay for a medical bill of less than $1,000.
- Two-thirds of those surveyed say they would shop around for the best price for medical care, and nearly half have delayed care due to concerns related to cost.
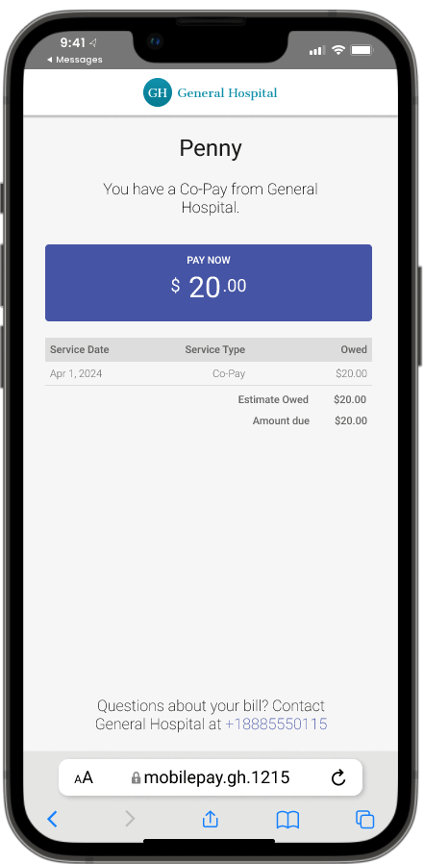
- About half of patients want to talk about payment options ahead of time, but 55% say providers don’t initiate those discussions.
- Consumers aren’t confident in how well they understand what’s covered in their health insurance plans. Twenty-eight percent said they understand which expenses are covered “a lot,” and 38% said they “somewhat” understand their coverage. Meanwhile, just 28% say they have discussed which healthcare expenses are and are not covered by their plan with a given provider.
The COVID-19 pandemic also disrupted healthcare organizations’ revenue cycle management practices. This past October, AccessOne interviewed healthcare revenue cycle executives about hospital revenue cycle KPIs and the impact of strategies used by hospitals and health systems to address this crisis. As providers acted swiftly to address the impact of the pandemic—and as revenue cycle staff shifted to a remote work environment—at some organizations, new strategies for handling billing statement and reimbursement disruption evolved. The impact:
- In some instances, any mention of COVID-19 on a patient record triggered an automatic hold on claim processing.
- By October, 50% of these hospitals and health systems still were feeling the impact of statement holds across multiple acute care settings.
- In addition, claims took five to 10 times longer to be reimbursed by insurance companies, which were also facing unknowns.
- Compounding this revenue disruption, point-of-service collections fell for all healthcare providers analyzed, while 43% of providers experienced an increase in requests and need for payment plans.
“Before the pandemic, it was clear that patients needed access to flexible payment options due to the rise in high-deductible health plans. COVID-19 exacerbated the issue with the increase in unemployment and loss of insurance coverage,” said Marvin Mickelson, System Director of Shared Revenue Cycle at The University of Kansas Health System. “We’ve focused on helping patients resolve their bills in a way that best suits their financial situation, whether by paying over a longer period of time or applying for financial assistance.”
The survey was commissioned by AccessOne and conducted by Engine Insights from Oct. 7-9, 2020. Engine Insights surveyed 1,004 people, and completed interviews were weighted by age, sex, geographic region, race and education to ensure reliable and accurate representation of the total U.S. adult population.
To see the full report, click here.